ASTM F640-23 Radiopacity Testing
Testing Services

ASTM F640-23
Radiopacity is the ability of a material to impede the passage of x-rays, thus making an object visible in an x-ray image. This allows for devices to be tracked in vivo during a medical procedure and identified if there is a part left behind. Radiopacity of a test article can be determined either qualitatively or quantitatively.
Qualitative radiopacity compares the visibility of a test article to a reference, such as a predicate device. Quantitative radiopacity calculates the difference in pixel intensity between the test article and the reference.
Evaluating the radiopacity of medical devices is important to the development process since it verifies that the device will be adequately visible during a procedure. Figure 1 shows an example of medical devices arranged on a phantom, which mimics a portion of the body during radiopacity evaluation.
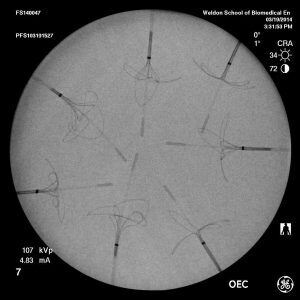
Figure 1. Sample of image used in radiopacity evaluation
Clinical Relevance
Radiopacity of medical devices is applicable in various clinical settings; the most prominent is fluoroscopy. Fluoroscopy is used for procedures in cardiology, gastroenterology, orthopedic surgery, and dental among others. During fluoroscopic procedures, clinicians have to consider the radiation dose to the patient and the operator from x-ray exposure, while obtaining images of sufficient quality.
Radiation dose, as well as image quality, can be altered by changing the settings for tube current and tube voltage of a c-arm fluoroscope. Tube current is measured in milliamperes (mA) and determines the amount of x-ray photons produced. If there are not enough photons, an x-ray image appears too grainy. Tube voltage is the energy of photons measured in kilovolts (kV) and determines the likelihood that the photons will be absorbed by the patient’s body. Additionally, the voltage affects image contrast between types of tissue composition. Increasing either current or voltage will increase patient radiation dose.
The patients’ physiology and health are other determinants for the c-arm settings. For thin patients, low current and voltage can be used. However for heavy patients, the voltage and current have to be increased to achieve a similar image quality. Additionally, settings vary for different parts of the body. Since image quality will always be further limited by “As Low as Reasonably Achievable” principles, resulting clinical images will rarely be 100% ideal. This means your devices will likely not be imaged under the most optimal settings for visibility in a clinical setting. Through the use of a mass-attenuating body phantom and clinically relevant imaging settings, we can provide a realistic representation of your device’s visibility.
Our Method
Our lab is ISO/IEC 17025:2017 accredited for radiopacity testing. We perform both qualitative and quantitative radiopacity evaluations in accordance with ASTM standard F640-23 and can accommodate other standards as needed for your device.
TEST METHODS
- ASTM F640
- ISO 4049
- Lab developed medical device testing method RAD-01
OUR COMMITMENT
We are committed to consistently performing services with high quality, that deliver exceptional results, and add value to the client’s business.
For client surveys sent since 2024, we received ratings of 4.99/5 (16).
